COLON CARCINOMA
Compiled by the APMG Molecular Committee- NORMAL MOLECULAR PATHWAYS AND ASSOCIATED MUTATIONS
- CLINICAL INDICATIONS FOR EGFR/KRAS/BRAF TESTING
- PROPOSED ALGORITHM FOR EGFR/KRAS/BRAF TESTING
- COMMENTS
- INTERPRETATION
- SUGGESTED READING
- GENETIC PATHWAYS
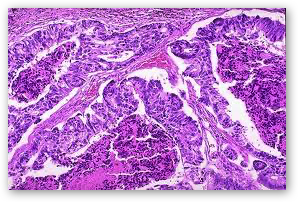
NORMAL MOLECULAR PATHWAYS AND ASSOCIATED MUTATIONS
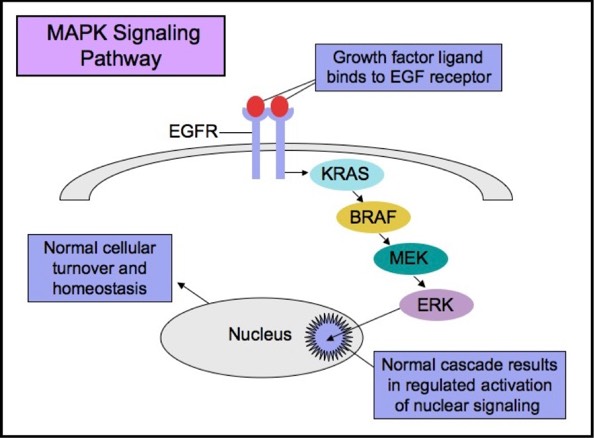
The RAS-RAF-MEK-ERK signaling pathway (MAPK pathway) is a classical intracellular pathway that plays a crucial role in homeostasis of normal cell turnover, cellular proliferation, differentiation, survival, and apoptosis. When activated aberrantly, this signaling pathway can induce tumorigenesis and has been associated with various malignancies.
MAPK Signaling Pathway
EGFR
The Epidermal Growth Factor Receptor (EGFR), also known as HER1 and ERBB1, is an important trans-membrane tyrosine kinase receptor involved in the initiation of the MAPK pathway. Activating mutations in EGFR can lead to aberrant cellular proliferation, inhibition of apoptosis, angiogenesis, increased cell survival, and gene transcription.
Some patients with tumors carrying EGFR mutations may respond to selective anti-EGFR therapies. EGFR has an extracellular ligand-binding region and a cytoplasmic tyrosine kinase-containing domain. Currently, there are two major types of anti-EGFR drug therapies. The first drug type (cetuximab, panitumumab) is a monoclonal antibody that inhibits EGFR by binding to an extracellular portion of the EGFR protein. The second type (gefitinib, erlotinib) is an intracellular tyrosine kinase inhibitor that inhibits EGFR by crossing the cell membrane and blocking the receptor’s active site.
Monoclonal Anti-EGFR Therapy
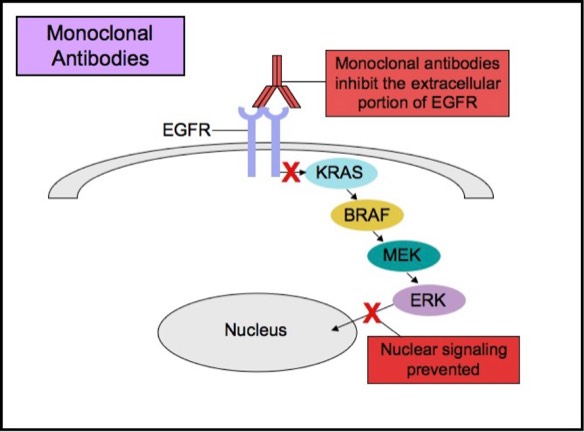
EGFR over-expression by immunohistochemistry is seen in approximately 80% of colon cancers. The overall significance of over-expression of EGFR in colon cancers is uncertain. Studies have shown that patients with or without EGFR over-expression often respond well to cetuximab. Therefore, cetuximab is now indicated for patients with colorectal cancer regardless of their EGFR status.
Research shows that EGFR over-expression does not actually translate into EGFR gene amplification or gene mutation. While EGFR over-expression is prevalent in colorectal cancers, EGFR gene mutations are not. Studies show that only a very small percentage of EGFR-positive colorectal cancers are associated with EGFR gene amplification. As a result, EGFR testing on colorectal cancers is not routinely performed.
Tyrosine Kinase Inhibitor Therapy
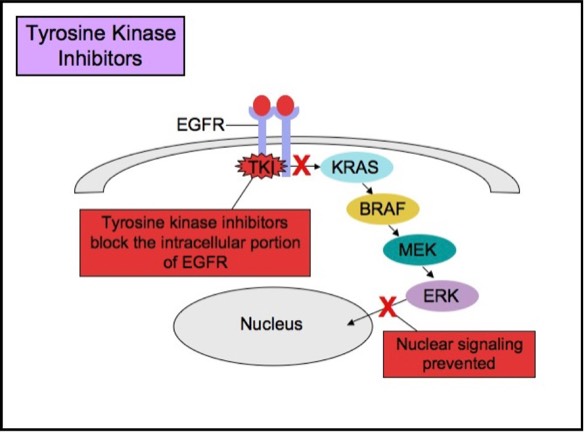
KRAS
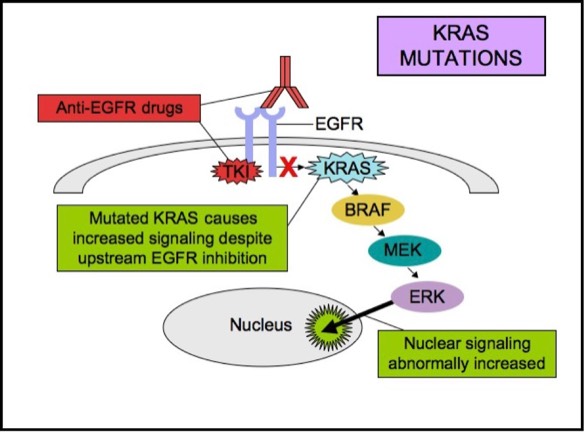
KRAS is a small G-protein that is important for EGFR signaling. About 40-50% of colorectal carcinomas harbor a KRAS mutation. KRAS mutation status has been extensively studied in colorectal cancers, as it is a strong predictive marker of resistance to anti-EGFR therapy. KRAS mutations activate downstream signaling cascade despite the upstream EGFR regulation. Anti-EGFR therapies are ineffective in tumors with such activating KRAS mutations, because the KRAS mutations trigger the EGFR-signaling cascade at a point downstream of the therapy’s target. Therefore, both monoclonal antibodies and tyrosine kinase inhibitors may fail to respond in the presence of KRAS mutations. Anti-EGFR therapies are less likely to be effective in patients with metastatic or advanced colorectal adenocarcinomas if a KRAS mutation is present.
KRAS Mutations
BRAF
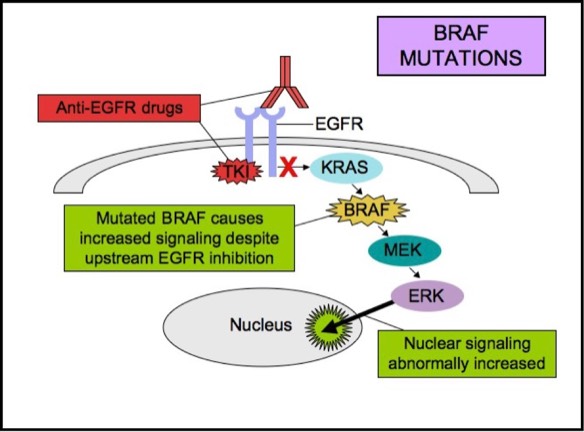
BRAF gene encodes a protein kinase, which is located downstream of both EGFR and KRAS in the MAPK pathway. BRAF mutations are seen in approximately 5 to 15% of all colorectal carcinomas. The most common mutation is BRAF V600E. BRAF mutations in colon cancer are associated with shorter overall survival. BRAF mutations are mutually exclusive of KRAS mutations, and similar to KRAS mutations, they also predict a lack of response to anti-EGFR therapies. Up to 15% of patients with KRAS wild-type metastatic colorectal cancer may show a BRAF mutation, which like a KRAS mutation, also may render anti-EGFR therapies ineffective.
BRAF Mutations
CLINICAL INDICATIONS FOR EGFR/KRAS/BRAF TESTING
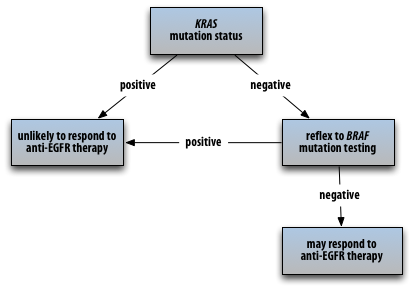
KRAS mutation analysis by polymerase chain reaction (PCR) in patients with colorectal adenocarcinoma may be ordered to identify patients who may or may not benefit from EGFR-directed therapies. Laboratories often offer KRAS mutation PCR test, with reflex to BRAF (if KRAS is negative), since the two mutations are mutually exclusive. EGFR testing (over-expression, gene mutation, gene amplification) for colon cancer is not routinely performed. When testing is desired, immunohistochemistry (IHC) is often used to evaluate EGFR protein over-expression, fluorescent in-situ hybridization (FISH) is typically used to detect EGFR gene amplification, and PCR is often employed to detect EGFR gene mutations.
Testing should be performed on:
- Patients with metastatic adenocarcinoma
- Patients with unresectable tumors
- Patients with recurrent tumors
- Patients who cannot tolerate conventional chemotherapy
Acceptable specimens usually include:
PROPOSED ALGORITHM FOR EGFR/KRAS/BRAF TESTING
While EGFR over-expression is prevalent in about 80% of colorectal cancers, EGFR gene mutations are not. As a result, EGFR mutation testing on colorectal cancers is not routinely performed. Anti-EGFR therapy is now indicated for patients with colorectal cancer regardless of their EGFR mutation status. However, determination of KRAS and BRAF gene mutation status is useful in identifying patients who are less likely to respond to anti-EGFR therapy. Both KRAS and BRAF mutations are associated with lack of a clinical response to anti-EGFR therapy. I am recommending (as available) KRAS testing with automatic reflex to BRAF testing if KRAS is negative to prevent clinicians needing to order the two tests separately. (Discussion with oncologists revealed that they usually prefer reflex testing to prevent having to re-order tests and subject the patients to insurance approval process a second time.)
TEST COMMENTS
KRAS and BRAF mutation analyses by PCR are available upon request. These tests are intended to detect KRAS or BRAF mutation-positive patients. Colorectal carcinomas with KRAS or BRAF mutations may show relative insensitivity to anti-EGFR therapies that target the RAS/RAF pathway.
TEST INTERPRETATION
PCR GENE MUTATION ANALYSIS INTERPRETATION:
Positive = Mutation Detected: Unlikely to respond to anti-EGFR therapy
Negative = Mutation Not Detected: May respond to anti-EGFR therapy
SUGGESTED READING
Krasinskas AM. EGFR signaling in colorectal carcinoma. Pathology Research International 2011.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3042643/
Sullivan KM, Kozuch PS. Impact of KRAS mutations on management of colorectal carcinoma. Pathology Research International 2011.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3062096/
CAP Colon Molecular Reporting Template
ALGORITHMS FOR LYNCH SYNDROME (COLON/ENDOMETRIAL CARCINOMA)
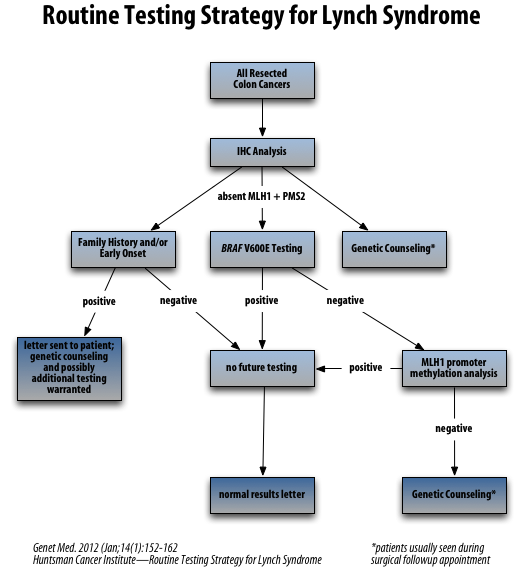
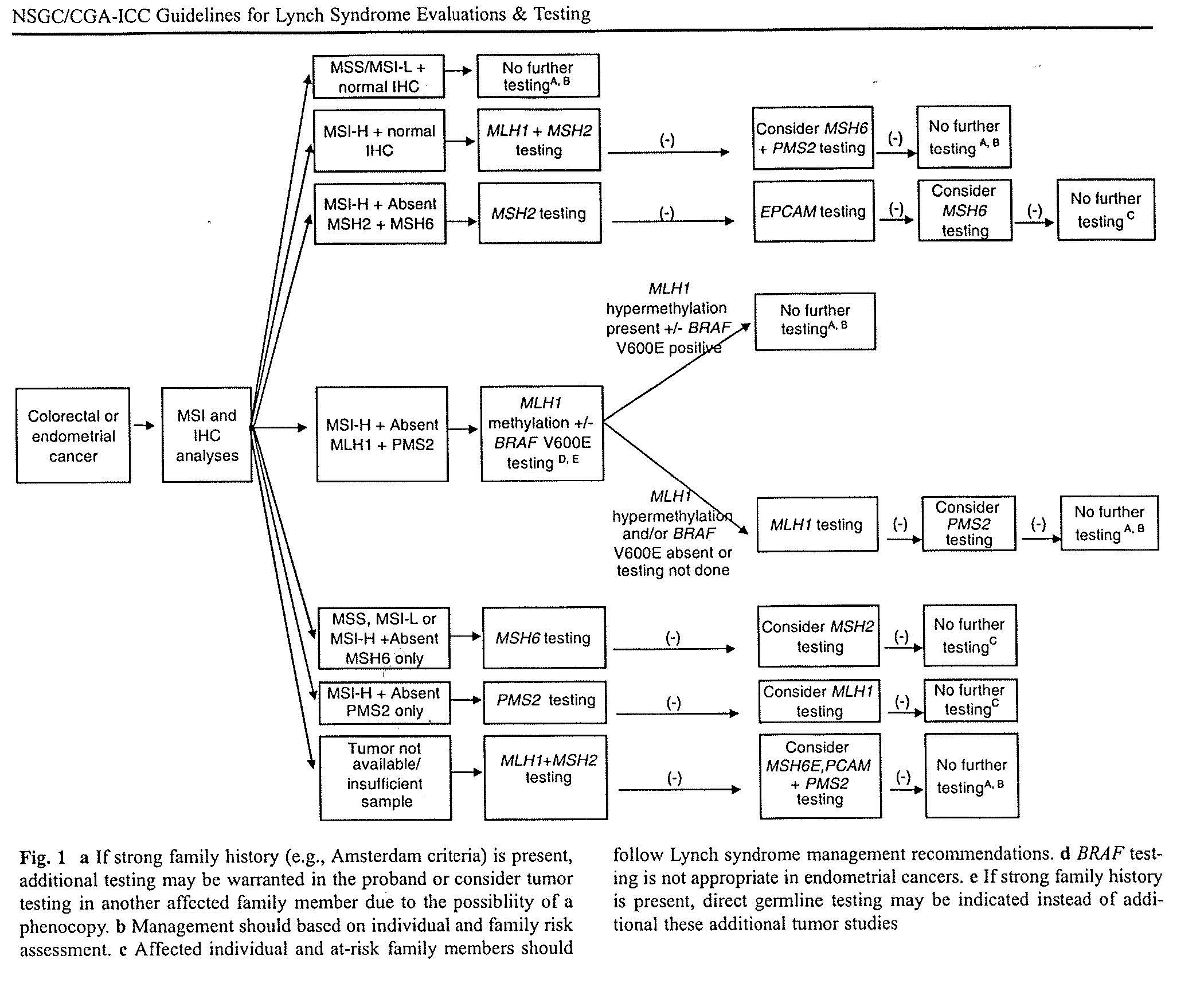
Reference: J Genet Couns. 2012 Aug;21(4):484-93


